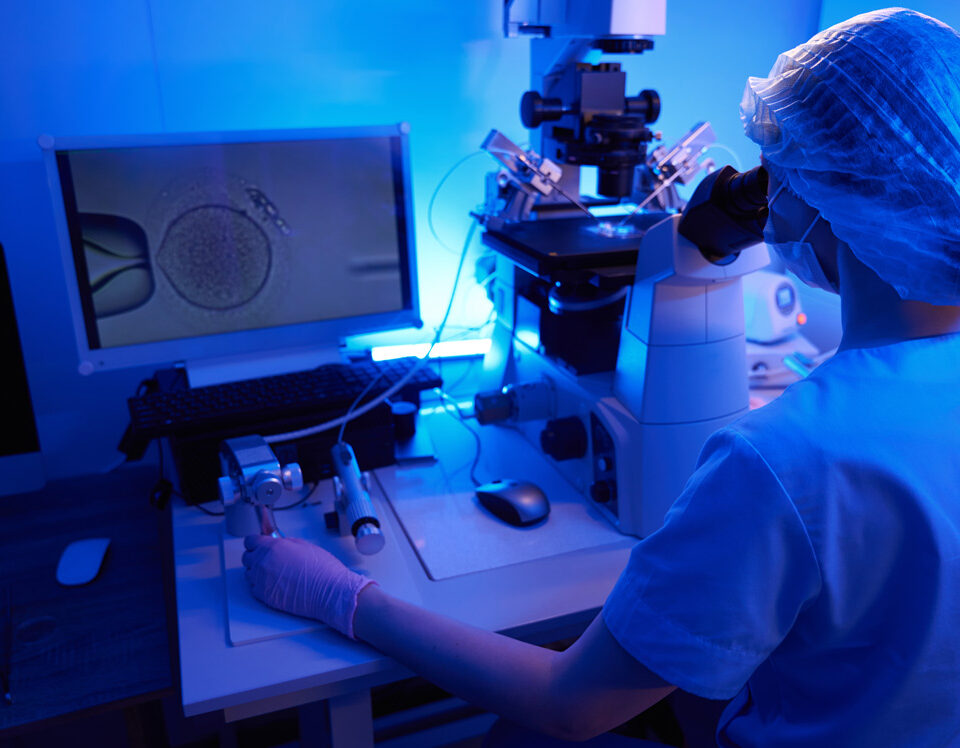
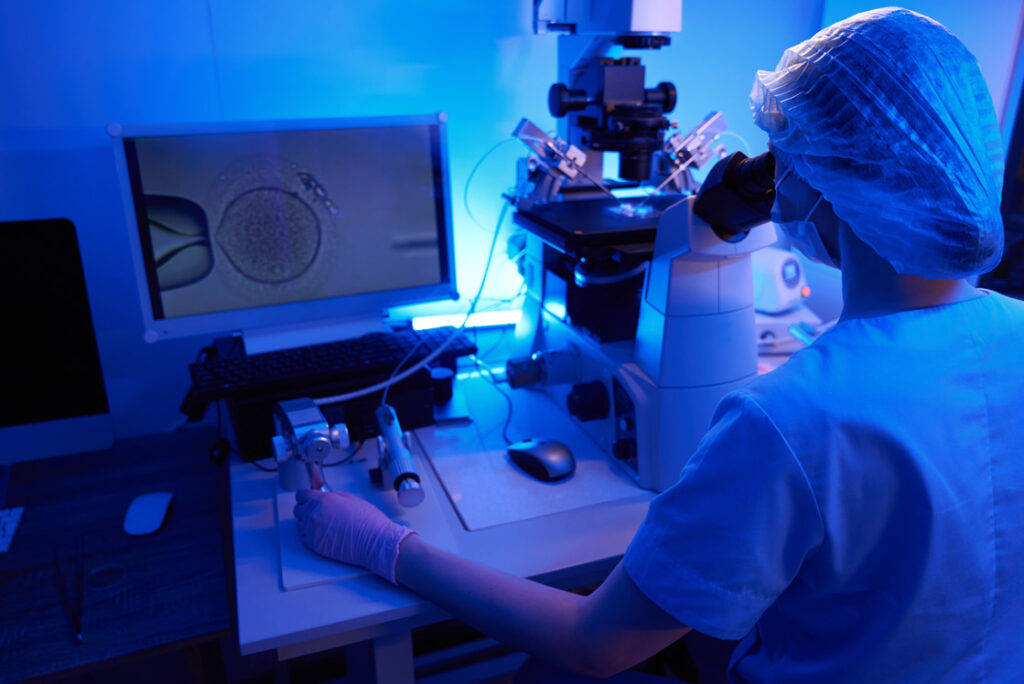
In-vitro fertilisation (IVF) and other fertility treatments help many couples and individuals achieve their goal of becoming parents. Embryology and IVF processes are highly specialised and rely on advanced science and technology – but they don’t need to feel confusing or inaccessible.
To make things clearer, we asked our expert embryologists, Mohsen Attia and Kyrillos Salib, to answer some of the questions we hear most often about what happens in our in-house laboratory. Kyrillos joined The Fertility & Gynaecology Academy in 2021. He plays a key role in our patient journeys, helping us deliver the highest standards of care.
How are embryos graded? Is grading the only factor when you select embryos for transfer?
Embryos are graded based on their appearance under the microscope. We look at factors such as cell number, symmetry, fragmentation on day three. For blastocysts (day five/six), we assess expansion, the quality of the inner cell mass and the trophectoderm.
Grading helps us understand how well an embryo is developing, but it is not the only factor we use when selecting embryos for transfer. We also consider the patient’s medical history, previous IVF outcomes, the genetic status of the embryo (if testing has been done), and how consistently the embryo has developed over time.
Good grading is reassuring, but embryos with slightly lower grades can still lead to healthy pregnancies. We have integrated AI embryo selection at The Fertility & Gynaecology Academy to empower our existing embryo assessment tools and improve outcomes.
What is PGT (genetic testing)?
Preimplantation Genetic Testing (PGT) is a technique used to analyse embryos for chromosomal or specific genetic conditions before transfer.
A few cells are gently removed from the embryo at the blastocyst stage and either sent to a specialist genetics laboratory, or tested in-house. The Fertility & Gynaecology Academy is one of the few fertility clinics in the UK which offers genetic testing in-house. PGT can identify chromosomal abnormalities, inherited conditions and the number of chromosomes present, helping reduce the risk of miscarriage and improving the chance of selecting an embryo with the best reproductive potential. It also helps prevent the transmission of genetic diseases from parents to their children.
Why don’t all embryos reach the blastocyst stage?
Embryo development is complex, and not every embryo will progress to the blastocyst stage. Several reasons explain why:
-
Genetic and intrinsic factors: Some embryos stop growing because of chromosomal abnormalities such as aneuploidy. These issues occur naturally and can result from poor egg or sperm quality, slow or irregular embryo development, or damage to mitochondrial DNA. Many of these factors are inherent to the embryo and cannot be influenced externally.
-
Extrinsic and environmental factors: Embryos are sensitive to their surroundings. Factors such as parental age can play a role, as chromosomal abnormalities become more common with advancing maternal or paternal age. In the laboratory, suboptimal conditions can affect embryo development. However, at The Fertility & Gynaecology Academy, we use time lapse imaging, meaning embryos remain in a stable environment throughout development, without being removed for assessment.
-
Biological function: Embryo arrest can be viewed as a natural protective mechanism. If an embryo stops developing, it is often because it would not have resulted in a viable pregnancy. Nature uses this process as a form of quality control.
Does embryo transfer on day 3 or day 5 offer a better chance of success?
The best timing varies between patients and depends on factors such as embryo number, quality and medical history. Both approaches can lead to successful pregnancies.
Benefits of day 5 (blastocyst) transfer
- Blastocysts have shown they can grow to a more advanced stage, which may improve selection.
- Higher implantation rates are often seen because the embryo is transferred at a stage more closely matching natural conception.
- Blastocysts allow better synchronisation with the endometrium.
Benefits of day 3 transfer
- Ideal when embryo numbers are low, giving embryos the opportunity to continue developing inside the uterus.
- May help avoid the risk of all embryos arresting in the laboratory.
- Suitable for patients with previous poor blastocyst development.
Why didn’t all my mature eggs fertilise?
Not all mature eggs will fertilise, even when conditions are optimal. Fertilisation depends on several factors, including egg quality, sperm quality, timing, and the way the egg and sperm interact during ICSI or standard IVF. Some eggs may appear mature but still lack the internal structures needed for normal fertilisation. Likewise, sperm may be unable to complete the fertilisation process even if they look healthy under the microscope. This variation is entirely normal in IVF and something we see frequently. The Fertility & Gynaecology Academy has the ability to address this issue using calcium ionophore.
Can we transfer a mosaic embryo?
Yes, mosaic embryos can be transferred, and they have resulted in healthy live births. When available, euploid embryos are prioritised first, as they have the highest implantation and live-birth rates and the lowest risk of miscarriage.
If no euploid embryos are available, low-level mosaic embryos are generally considered next, followed by high-level mosaic embryos, after appropriate counselling.
The decision to transfer a mosaic embryo should always involve detailed genetic counselling, discussion of potential risks, and consideration of embryo-specific findings.
How long can frozen embryos be stored?
In the UK, frozen embryos can be stored for up to 55 years, provided consent forms are renewed at the required intervals every 10 years. Advances in vitrification techniques allow many embryos to maintain long-term viability by protecting them during the freezing process.
What is the chance of an embryo not surviving the thaw?
The majority of embryos survive the thawing process, particularly when vitrification is used. Our embryo survival rate exceeds 95%*. An embryo is considered to have survived thawing if 50% or more of the embryo remains intact after thaw. At The Fertility & Gynaecology Academy, the vast majority of thawed embryos retain more than 95% of their total embryo volume.
You can read more about how to increase frozen embryo transfer success in our helpful article.
* These figures have been retrieved from clinic data for the year 2020-2025
Can I do anything to improve my egg or sperm quality?
While age and biology play a major role, lifestyle changes can support reproductive health.
For improving egg quality
- Eat an antioxidant-rich diet – Include foods such as berries, leafy greens and whole foods.
- Avoid smoking, excess alcohol and other harmful substances.
- Manage stress and prioritise rest and self-care.
For improving sperm quality
- Adopt a healthy lifestyle with regular exercise.
- Eat a balanced diet, including antioxidants and healthy fats.
- Avoid prolonged heat exposure, such as hot tub and sauna use, or using a laptop on your lap.
- Manage stress levels.
- Limit exposure to environmental contaminants.
Want to take the next step in your fertility journey?
Understanding what happens behind the scenes when it comes to embryology and IVF can make your fertility journey feel far less overwhelming. As Kyrillos explains, every embryo is assessed with precision, every development step is monitored with care, and each decision is guided by both science and compassion. Whatever stage you’re at in your fertility journey, having clear information puts you in control.
If you’re ready to take the next step, our experienced team is here to support you with advanced testing and evidence-based fertility care. We’d be happy to talk to you about our experience, specialist areas, and success rates.
Book a consultation today to discuss your options and begin your path forward with confidence. Call 020 7224 1880 or email us at info@fertility-academy.co.uk