You might be wondering ‘Why does IVF fail?’. We have heard many success stories about in-vitro fertilisation (IVF) treatments from friends, family or on the internet. However, it’s not often that we hear about failed IVF, usually because it is a very emotional subject for those who are aspiring to be parents. This blog post serves to break the taboo and cover some of the reasons why IVF might fail.
Our latest success rates, as submitted to the Human Fertilisation and Embryology Authority (HFEA), indicate that our IVF treatment has a clinical pregnancy success rate of 40.6% and a live birth rate of 32.5%. When it comes to patients that do not achieve a clinical pregnancy or live birth, there are a number of reasons why their IVF has been unsuccessful.
Female age
As women grow older, their eggs decrease in quality and quantity. It’s well known that women have less chance of becoming pregnant as they age due to this fact; however, a decline in egg quantity and particularly quality also affects the chances of a clinical pregnancy or live birth through IVF treatment.
Dr Gorgy, co-founder of The Fertility and Gynaecology Academy, and one of the UK’s most respected fertility consultants, says, “According to our success rates, women up to the age of 35 have the highest chance of IVF success: 47% for clinical pregnancy and 38% for live birth.”
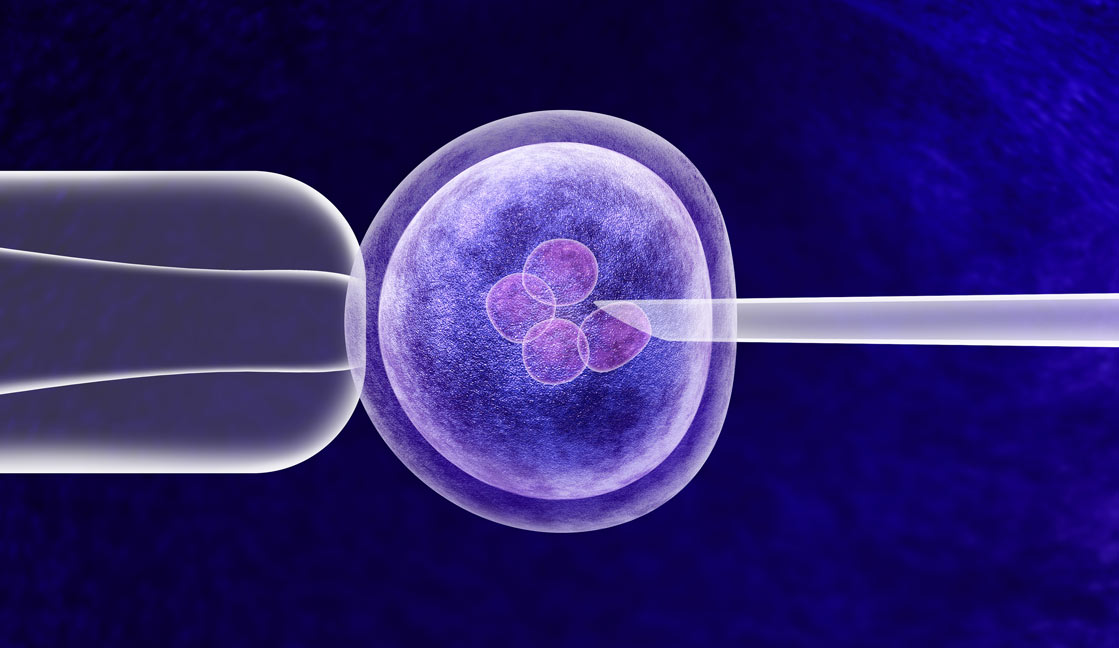
Embryo quality
During the laboratory portion of IVF treatment, the female’s eggs and the male’s sperm are mixed together with the aim of creating an embryo. Embryos can appear healthy in the lab, but when implanted into the uterus there is a possibility that they fail to implant due to an invisible defect. Our IVF Lab uses a score system to grade the quality of the embryos and choose the best to be put back into the uterus. We also use time-lapse imaging (embryoscope) to incubate the embryos until the blastocyst stage (5 day old embryos). The embryoscope is a closed incubator with a camera inside that takes photos of the embryos every 10-20 minutes. We can watch the progress of the embryos through the screen on the outside of the embryoscope and therefore we do not need to take the embryos out each day to assess them, which keeps them in a stable environment. We can also rewind the video recording and assess the development of the embryos overnight, enabling us to choose the best for the embryo transfer to achieve pregnancy.
Ovarian response
In the beginning of IVF treatment, the female is required to administer a daily injection of a fertility hormone called follicle stimulating hormone (FSH), which aims to increase egg production. Some women’s ovaries do not respond correctly to this medication and thus fail to produce multiple eggs for collection. This is especially true in older women due to the already low quantity of eggs (low ovarian reserve).
Dr Gorgy says, “If a poor ovarian response happens, it doesn’t mean it’s the end of the IVF treatment. Investigations and alterations to medication may be able to amend the situation. The ovarian reserve is assessed with a blood test for the Anti-Mullarian Hormone (AMH) and an ultrasound scan looking at the antra follicle count. The ovarian reserve would determine the best protocol and dose of the hormone to stimulate your ovaries and produce a reasonable number of eggs.”
Implantation issues
This means that the embryos failed to implant in the uterus. This could be because of the presence of uterine polyps, a premature increase in progesterone levels, an endometrial lining that is too thin, or an infection of the uterus. “It is not your fault if an embryo fails to implant,” Dr Gorgy says, “most of the time, implantation issues are beyond anyone’s control. We gather a comprehensive group of tests to check for the possible causes of implantation failure”.
Lifestyle
As with a natural pregnancy, maintaining a healthy lifestyle before and during IVF is likely to help conception. If you smoke, it is wise to quit a few months before you begin IVF, as smoking is shown to negatively impact fertility. Achieving a healthy weight will also benefit you, as well as maintaining a nutritious diet and exercising regularly.
Chromosomal abnormalities
IVF can fail due to embryos that have chromosomal abnormalities. This means that the embryo has a missing, extra, or irregular portion of chromosomal DNA. The body then rejects the embryo and this results in IVF failure. Chromosomal abnormalities could be inherited from one of the parents or be newly developed during the early stages of the embryo division.
Dr Gorgy says, “Chromosomal abnormalities are most likely to be present in the embryos of women over the age of 35. However, don’t let this put you off. We can test the embryos for all 23 pairs of chromosomes for any inherited chromosomal or gene abnormalities and replace only the normal embryos.”
Reproductive immunology is the theory that an embryo or fetus is rejected due to over-active immune cells in the body. If you have gone through IVF cycles but you have failed to give birth, there is a possibility that your immune cells could be attacking the embryo. Reproductive immunology could offer some insight into why your IVF cycles have recurrently failed and, if your immune system is reacting in this way, provide a treatment plan.
Why does IVF fail?: Reducing the risk of repeat IVF failure
It does sometimes take two or more cycles of IVF to achieve a successful outcome. While this can take its toll on you physically, emotionally and mentally, it may help to know that you are not alone in your struggle, that there is help available from fertility experts with decades of experience, and that IVF failure is not your fault.
With each cycle of IVF, your doctor will advise on what caused the failure, and how to use this information to improve your chances of success if you do decide to undergo IVF again. A few of the assessments which can be performed to get to the root of the IVF failure include:
If you have any further questions, our embryologists and physicians will be happy to assist. Simply call the clinic on 020 7224 1880, or to book a consultation online, click here.