If you’ve experienced failed fertility treatment, or you are about to begin your IVF journey, you may be wondering, “what is the biggest cause of IVF failure?”
The truth is, IVF is a complex process with many moving parts, and can fail for a number of reasons, such as the quality of the eggs and sperm used in the treatment, genetic abnormalities, implantation issues and underlying conditions such as endometriosis.
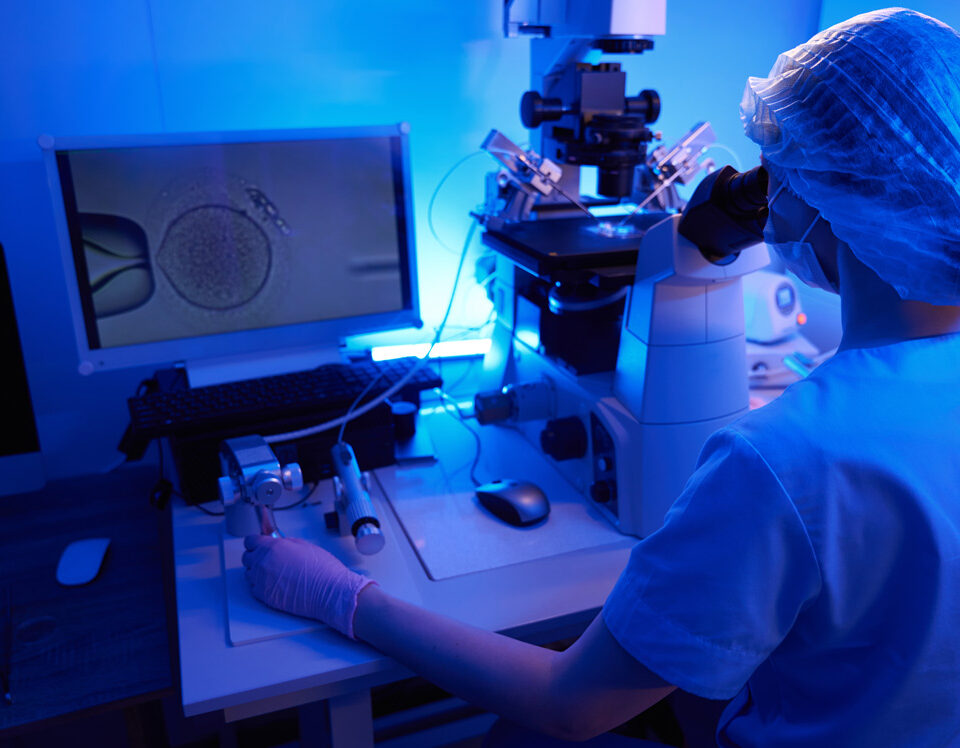
Determining the cause of failed IVF requires rigorous fertility testing, and as specialists in recurrent IVF failure and recurrent miscarriage, we are equipped with the knowledge and advanced technology to diagnose and treat complex cases. As Dr Gorgy, Co-Director and Fertility Consultant at The Fertility & Gynaecology Academy, explains, “The key to successful IVF is identifying and addressing any underlying causes that may be reducing your chances of success. At The Fertility & Gynaecology Academy, we take a personalised approach to every patient. By thoroughly investigating and optimising each step of the treatment process, we give patients the best possible chance of success.”
What’s the success rate for IVF?
When it comes to IVF, success can be measured in different ways. The pregnancy rate refers to the number of confirmed pregnancies after treatment, while the live birth rate tracks how many of those pregnancies result in a live baby.
Comparing clinic success rates can help you understand what to expect, but it’s important to bear in mind that figures are influenced by the types of patients a clinic treats, including age, diagnosis and medical history.
Our own success rates reflect a commitment to high quality treatment and advanced techniques. But even with excellent care, IVF is never guaranteed. Understanding why IVF might fail can help you prepare for the next step.
Common reasons for IVF failure
Uterine factors
The uterus must be optimal condition for an embryo to implant successfully. If the endometrial lining is too thin or not responding as expected, implantation may fail. Treatments like endometrial rejuvenation could help improve endometrial thickness and receptivity.
Sperm quality
Even if sperm counts look normal, DNA fragmentation or other abnormalities can affect fertilisation and embryo development. Sperm testing beyond the basic semen analysis can uncover issues not seen in standard tests.
Chromosomal abnormalities
One of the most common causes of IVF failure is chromosomal abnormalities in embryos. These can happen naturally, especially as maternal age increases. Preimplantation Genetic Testing for Aneuploidy (PGT-A) can be used to screen embryos before transfer.
Egg and embryo quality
Egg quality declines with age, but other factors such as ovarian reserve, stimulation protocol and genetics also play a role. Poor-quality embryos may fail to develop or implant properly.
Age of the mother
The age of the woman undergoing IVF has a direct impact on success. Fertility begins to decline in a woman’s thirties and more steeply after the age of 35.
Ovarian response
If the ovaries don’t respond well to stimulation drugs, fewer eggs will be retrieved, and this can limit chances of IVF success. Adjusting medication protocols in future cycles can often improve the response.
Implantation issues
Even when a healthy embryo is transferred, implantation doesn’t always occur. This may be due to immune system issues, undiagnosed uterine abnormalities or inflammation.
So, what is the most common reason?
Poor embryo quality is thought to be the most common cause of IVF failure. This is usually due to the embryo not developing properly, or having chromosomal abnormalities that prevent implantation or result in an early miscarriage.
Is my clinic to blame for IVF failure?
It’s natural to feel frustrated when IVF fails, and you may wonder if your clinic could have done more. In many cases, however, failure is not due to error or poor practice (fertility clinics in the UK carry out IVF and other fertility treatments very regularly, and are highly regulated by HFEA). Rather, it’s most likely the result of other factors which need to be investigated.
However, if you feel that your clinic isn’t offering answers or tailoring your treatment plan, it may be worth seeking a second opinion.
Can I help prevent IVF failure?
You can take some steps to improve your chances of IVF success, but it’s important to remember that even when you do everything right, IVF can still fail. Here are some lifestyle factors that may make a difference:
- Stop smoking: Smoking negatively impacts fertility in both men and women.
- Maintain a healthy weight: Being over or underweight can affect hormonal balance and IVF outcomes.
- Consume a balanced diet: Focus on whole foods, lean protein and a range of fruits and vegetables.
- Reduce stress: Stress alone is not a cause of IVF failure, but managing it can contribute to balanced hormones and allow you to better cope with treatment.
- Exercise gently: Regular movement can support hormone regulation, but avoid overexertion during treatment.
IVF failure usually indicates the need for further testing or a change in approach – not that anything is ‘wrong’ with you.
What to do if IVF fails
First, give yourself space to process. IVF failure is emotionally and physically exhausting. When you’re ready, you may wish to:
- Consult with your fertility specialist, who can advise on the most appropriate next steps for you
- Consider further testing, such as immune testing or genetic screening
- Explore different treatment options, such as a different stimulation protocol or medication tweak; using donor eggs or sperm; endometrial and ovarian rejuvenation; surrogacy; or other assisted reproductive techniques
At The Fertility & Gynaecology Academy, we believe that every fertility journey deserves a personalised approach. If your IVF has failed, or you’re starting treatment for the first time, we’re here to offer expert guidance and compassionate care.
Call 020 7224 1880 or email info@fertility-academy.co.uk to contact our friendly reception team and book a consultation.